How it works
Decode your body in as fast as 7 days and track ongoing progress
Step 1
Test what matters
Advanced testing of up to 150 biomarkers with results in 7 days or less. Convenient options for at-home or in-clinic blood collection.
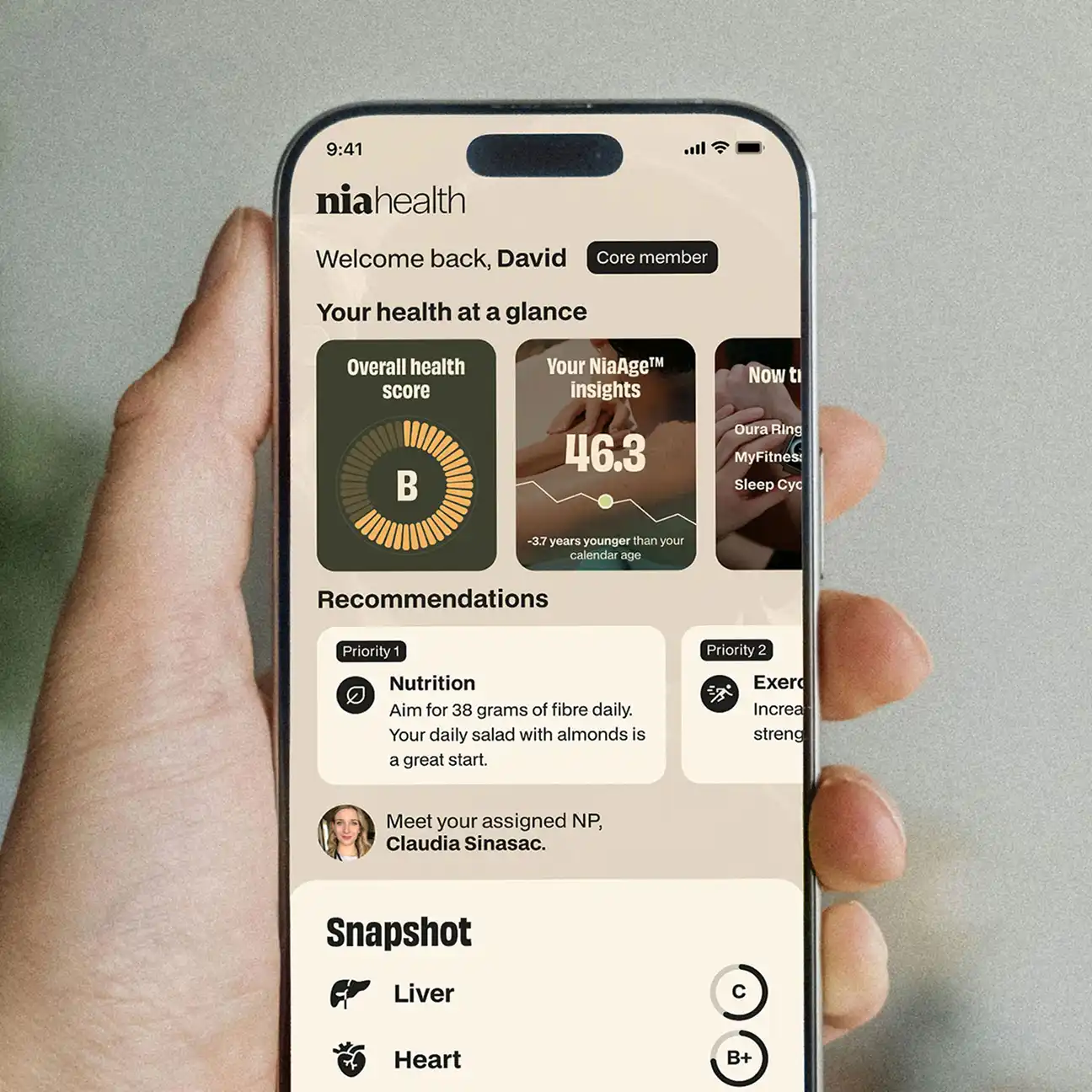
Step 2
Understand your action plan
Get your hyper-personalized action plan handwritten by a Canadian clinician (not generic AI). Unrushed virtual consultations available any time.

Step 3
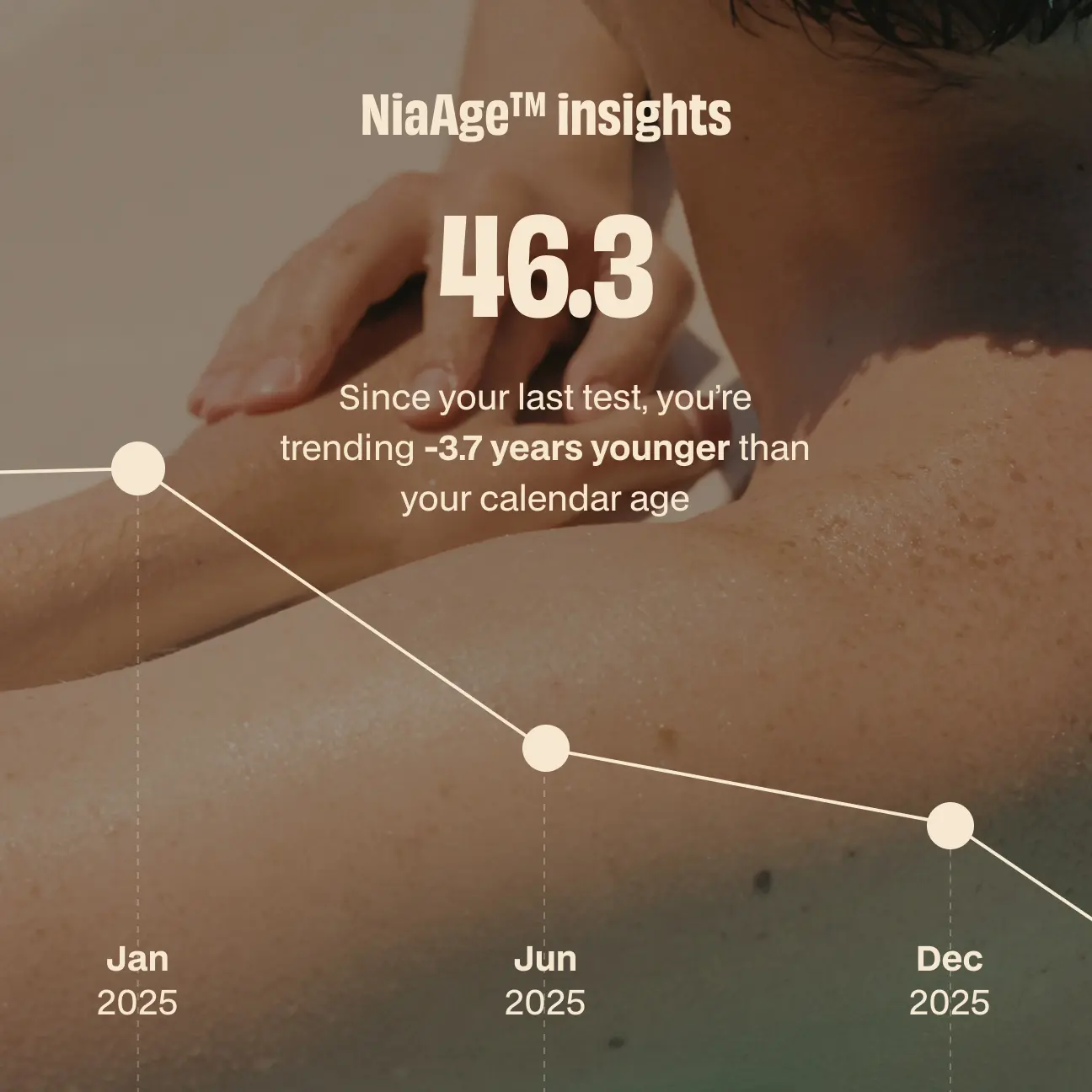
Track real progress
Test again each year with your clinician by your side. Integrate your wearables and health apps for deeper insights.
Included in all plans:
FAQ
Still have questions?
NiaHealth currently operates in Alberta, British Columbia, Manitoba, New Brunswick, Newfoundland and Labrador, Nova Scotia, Ontario, Prince Edward Island, and Saskatchewan.
No - we do not prescribe medication. However, we do provide, where applicable, suggestions. For interventions (including medications and supplements), we include a note of suggestions that you can discuss with your current medical team. Prescriptions are left to their discretion.
We offer advice to enhance your current health state, emphasizing prevention through exercise, nutrition, sleep, and emotional well-being but not medical management of existing illness. If we discover any incidental health issues, we provide suggestions for discussion with your primary care provider. While our suggestions impact overall health and various chronic conditions, comprehensive medical management of existing illnesses remains the responsibility of your current medical team.
It isn't an absolution you cannot do NiaHealth for one year after pregnancy. Here is the nuance: NiaHealth isn’t designed for use during pregnancy as pregnancy brings big changes to your hormones, metabolism, and other body systems. These shifts make it hard to interpret biomarker data accurately. During pregnancy, your healthcare team is the best source for lab testing—they’ll focus on the specific markers that reflect the health of both you and your baby.
It is your choice as to when you have your next NiaHealth draw after pregnancy. After birth, your body goes through a recovery phase often called the “fourth trimester.” During this time, your hormones and metabolism gradually start returning toward their usual patterns. Many people notice things begin to stabilize around three months postpartum, though everyone’s timeline is a bit different.
If you’re breastfeeding, your body will continue to experience changes. Because of this, it can take longer for your system to fully settle. Between about three months and up to a year after delivery, your results from any biomarker-based health tools—including NiaHealth—can still fluctuate. By around one year postpartum, many people’s biomarkers are closer to their baseline, which makes results more reliable for understanding long-term health patterns.
No. NiaHealth does not sell your personal health information to third parties. NiaHealth has not and will not engage in the sale of personal health information for monetization purposes. If you have any questions, please review our Privacy Policy or reach out to our Chief Privacy Officer at privacy@niahealth.co.
Your blood. Your data. Your move.
