Know your body. Change your future.
Test up to 10x more biomarkers than standard checkups, with hyper-personalized human clinician guidance. From $299/yr.

What do I get with a NiaHealth annual membership?
Go beyond just testing, with hyper-personalized plans from longevity-trained clinicians
Numbers
We test your biomarkers, and collate them with your wearable and health app data.
Interpretation
Our clinicians connect this data with your health story for a report tailored to your age & gender.
Actions
Get a hyper-personalized action plan that fits real life… leading to real progress.
Health
Numbers + Interpretation + Action = Health. And that's why we're called NiaHealth.

Health isn’t a snapshot. It’s a story. And you get to write what happens next.
Built for every kind of curiosity

You want to optimize for peak performance
You already track your sleep and exercise. Now get advanced data for precision protocols.

You’ve had a wake-up call or life shift
Turning 40? New parent? Recent health scare? Get a plan to stay healthy longer.

You want answers—and to feel heard
Unexplained fatigue? Not feeling seen? Our clinicians dig deeper, listen longer.
One test.
Early detection of 1,100+ risks.
Don't wait for symptoms. Know and reverse risk years in advance.
We don't just test. Hyper-personalized plans to change your trajectory.
71
Uncovered a hidden risk that was actionable
18
Detected genetically linked heart disease risk
51
Reversed early signs of diabetes within a year
63
Improved their biological age within a year
Not just a blood test.
A plan as unique as your body.
Hyper-personalized guidance from Canadian clinicians—add life to your years, and years to your life

eGFR kidney function

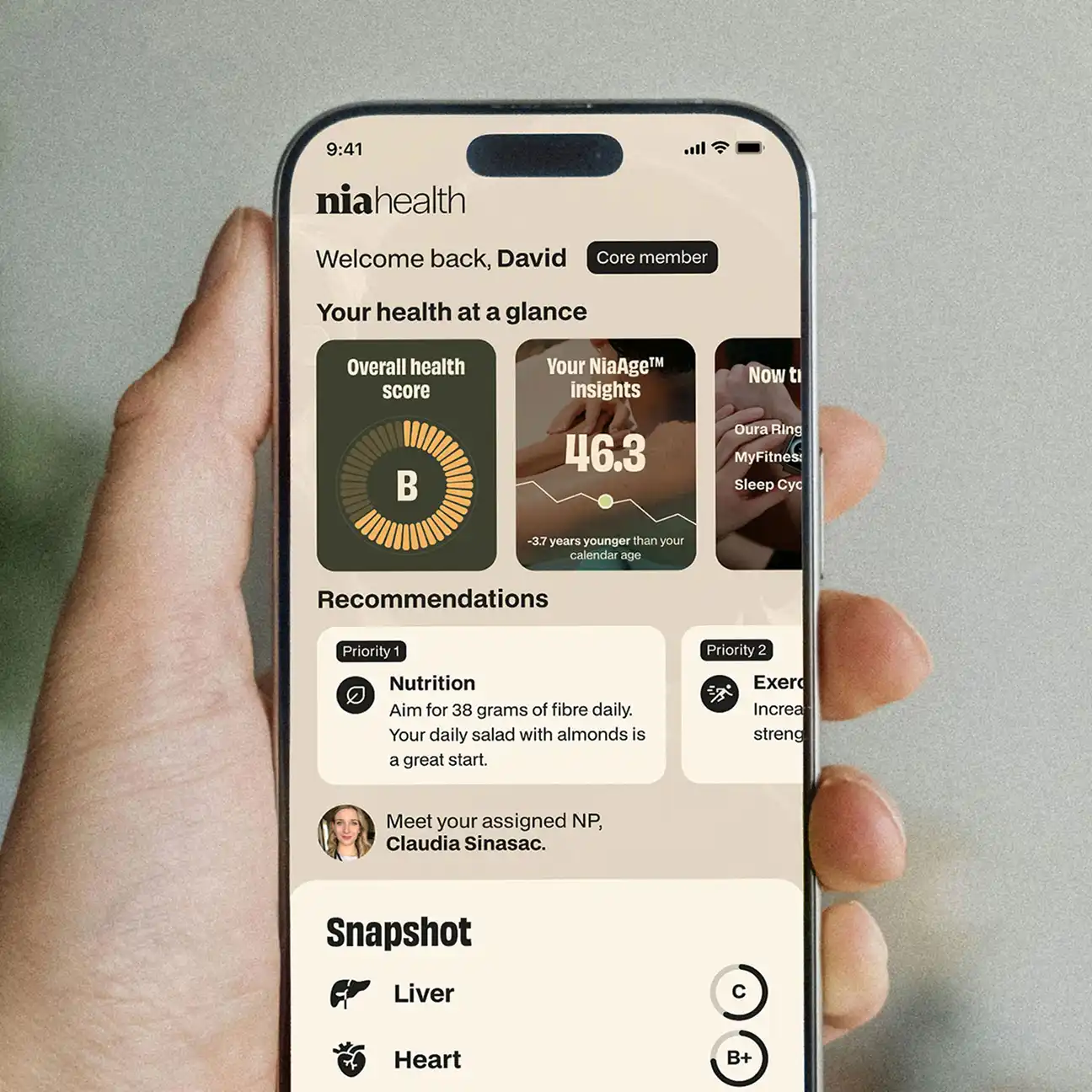
Overall health score


Your NiaAge

Your LDL-c is suboptimal for your age and gender, and with your family history, it's key to take steps to reduce your risk. Here is your action plan.
How it works
Health advice without the jargon or judgement—just simple, science-backed clarity that actually works
Test what matters
Advanced testing of over 150 biomarkers with results in 7 days or less. Convenient options for at-home or in-clinic blood collection.
Data informs actions
Get your hyper-personalized action plan handwritten by a Canadian clinician (not generic AI). Unrushed, shame-free 1:1 virtual consultations available any time.
Track real progress
Test again each year with your clinician by your side. Integrate your wearables and health apps for deeper insights. Explore demo dashboard →


Data you can trust. Privacy you can count on.
Your health data is encrypted, stored in Canada, and protected by military-grade security, fully aligned with PHIPA, HIA, and PIPEDA standards, and overseen by our Chief Privacy Officer under an ironclad privacy policy.

We're not replacing your doctor.
We're filling the gaps.
We do the deep, preventive testing that most checkups miss.
Find your perfect annual plan
Start with Core—our most popular plan with a signature virtual clinician consult
Core
Includes:
- 60 total biomarkers tested
- Hyper-personalized health plan written by Canadian clinicians
- Longevity risk by decade
- 1:1 signature virtual clinician consult
- NiaAge biological age
- Exclusive early access to new features
- Unlimited SMS Q&A support
All plans include:
Built by Canadians. Right by Canadians.
See what's humanly possible
FAQ
Still have questions?
NiaHealth currently operates in Alberta, British Columbia, Manitoba, New Brunswick, Newfoundland and Labrador, Nova Scotia, Ontario, Prince Edward Island, and Saskatchewan.
No - we do not prescribe medication. However, we do provide, where applicable, suggestions. For interventions (including medications and supplements), we include a note of suggestions that you can discuss with your current medical team. Prescriptions are left to their discretion.
We offer advice to enhance your current health state, emphasizing prevention through exercise, nutrition, sleep, and emotional well-being but not medical management of existing illness. If we discover any incidental health issues, we provide suggestions for discussion with your primary care provider. While our suggestions impact overall health and various chronic conditions, comprehensive medical management of existing illnesses remains the responsibility of your current medical team.
It isn't an absolution you cannot do NiaHealth for one year after pregnancy. Here is the nuance: NiaHealth isn’t designed for use during pregnancy as pregnancy brings big changes to your hormones, metabolism, and other body systems. These shifts make it hard to interpret biomarker data accurately. During pregnancy, your healthcare team is the best source for lab testing—they’ll focus on the specific markers that reflect the health of both you and your baby.
It is your choice as to when you have your next NiaHealth draw after pregnancy. After birth, your body goes through a recovery phase often called the “fourth trimester.” During this time, your hormones and metabolism gradually start returning toward their usual patterns. Many people notice things begin to stabilize around three months postpartum, though everyone’s timeline is a bit different.
If you’re breastfeeding, your body will continue to experience changes. Because of this, it can take longer for your system to fully settle. Between about three months and up to a year after delivery, your results from any biomarker-based health tools—including NiaHealth—can still fluctuate. By around one year postpartum, many people’s biomarkers are closer to their baseline, which makes results more reliable for understanding long-term health patterns.
No. NiaHealth does not sell your personal health information to third parties. NiaHealth has not and will not engage in the sale of personal health information for monetization purposes. If you have any questions, please review our Privacy Policy or reach out to our Chief Privacy Officer at privacy@niahealth.co.
Data you understand. Human guidance you can trust. Results you notice.